Organ Transplantation in Iran
An organ transplant refers to the medical procedure in which a diseased organ is replaced by a healthy organ. It is done in cases that a patient suffers from severe organ failure and needs to consider organ transplant surgery. The organ may be from a living donor, or from a donor who has suffered a life-ending accident.
Receiving a new organ is a life-saving and yet complicated process. Once you are diagnosed with organ failure, you will be referred to an organ transplant center, and will be placed on the waiting list for organ transplant.
In some cases, the donor can be a family member or a friend or in rare cases a person not related to the receiver of the organ. This type of organ donation is called living organ donation.
It is noted that people can register as an organ or tissue donor anytime at their convenience, and their organs would be used in case they are brain dead. It is also noteworthy that (even in cases of accidents that could lead to severe injuries like brain death) doctors have taken oaths to do no harm and place saving a patient’s life above anything.
Once consent is granted by the donor or the donor’s family, the organ and tissue transplant can take place. When any organ and tissue are recovered, OPU (Organ Procurement Unit) finds a suitable match for someone on the organ and tissue transplant waiting list.
It is of high importance to note that according to the Iranian Medical Law concerning transplantation for foreigners, the donor should also be a foreigner.
Here is a brief explanation on different types of organ transplant.

Heart Transplantation
While a patient, who is suffering from end-stage heart failure or severe coronary artery disease, is waiting for a transplant he or she may need surgery to place an LVAD (Left Ventricular Assist Device) to temporarily improve heart function.
Since heart transplantation is a complex procedure, the medical team imposes strict medical criteria in assessing whether a donor’s heart is suitable for transplant, and whether a potential recipient is suitable to receive the transplant.
In this procedure, a healthy heart from a brain-dead donor is used to replace a patient’s damaged or diseased heart.
It is noteworthy that about 100 heart transplantations are yearly carried out in Iran, and the first heart transplantation in Iran took place in November 1969.

Dialysis and Kidney Transplantation
There are different causes for kidney failure, but dialysis allows patients to tolerate the wait for an organ.
It is noted that kidney transplantation is the most needed and transplanted organ, and more than 2,500 kidney transplants are yearly carried out in Iran. It is also noteworthy that the first kidney transplantation in Iran took place in November 1968.
In this procedure, a healthy kidney from a dead or living donor is replaced with the patient’s diseased kidney.
Diabetes and Pancreas Transplantation
Pancreas transplantation involves implanting a healthy pancreas into a person who suffers from diabetes, since in type 1 diabetes due to some permanent damage, pancreas is not able to produce insulin anymore.
The purpose of this procedure is to produce complete insulin independence, and in some cases it may also treat type 2 diabetes.
In this procedure, the healthy pancreas from a brain-dead donor or a partial pancreas from a living donor is replaced with the damaged one.
It is noteworthy that since uncontrolled diabetes can lead to kidney damage, pancreas transplantation may prevent the need for kidney transplantation in the future.

Liver Transplantation
Liver failure has different causes, including cirrhosis, and its only treatment is liver transplant, also called hepatic transplantation.
In this procedure a healthy liver graft from a donor is replaced with the patient’s diseased liver. Liver graft can be from a brain-dead donor or a family member.
Lung Transplantation (Pulmonary Transplantation)
Several factors including COPD (Chronic Obstructive Pulmonary Disease) lead to lung failure and the need for lung transplantation. Lung Transplantation, also called Pulmonary Transplantation, is used for people whose conditions are so severe that other treatments no longer work.
In this procedure the patient’s diseased lung is partially or totally replaced with a healthy lung from a brain-dead donor.
In some conditions two lungs may be transplanted at the same time.
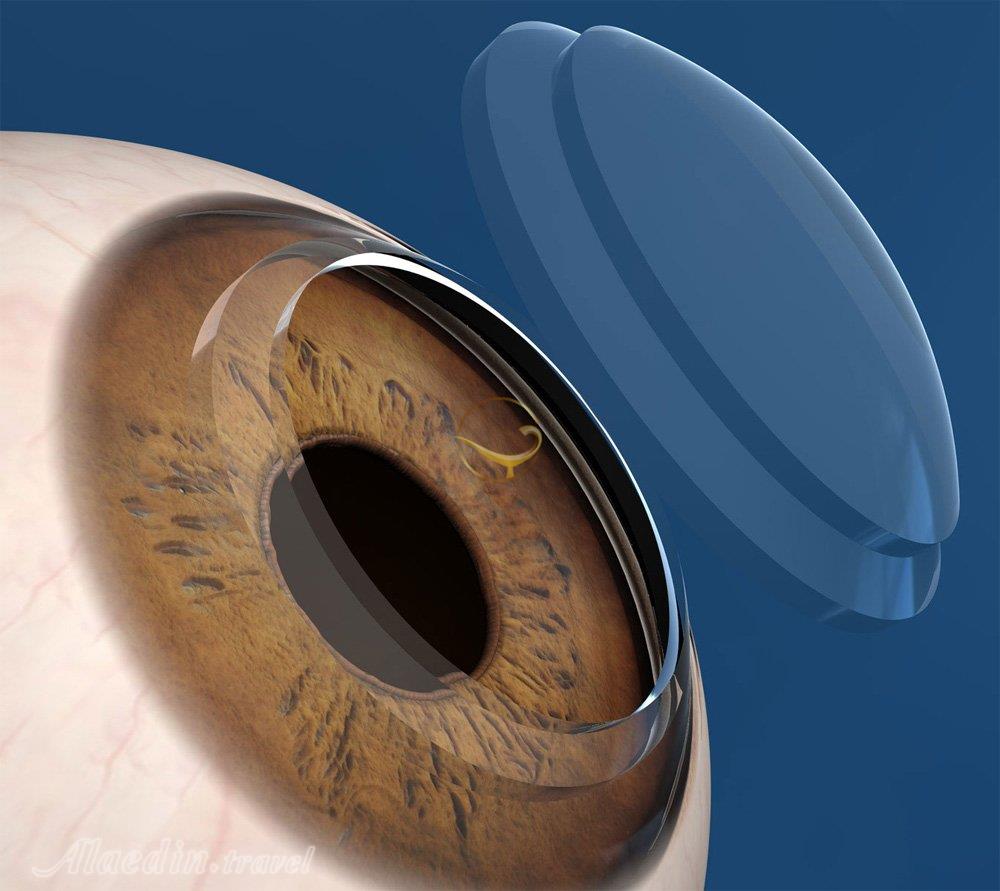
Cornea Transplantation
Corneal transplantation, also known as Penetrating Keratoplasty, is a surgical procedure for replacing damaged or diseased cornea by a healthy donated corneal issue. Since clear cornea is essential for vision, it is important to have corneal transplantation.
It is noted that corneal donation restores vision to those blinded by corneal disease, which is the fourth most common cause of blindness.
The procedure takes up to 2 hours, and is performed under local anesthesia with injection around the eye to relax the muscles that control blinking and eye movement. Then your surgeon measures the affected corneal area to determine the size of the needed donor tissue, and then positions and sutures it into place.
To improve vision and clarity sometimes LASIK is suggested after cornea transplantation. Your surgeon may also prescribe steroid eye drops to help your body accept the new corneal graft.
The recovery time takes several weeks up to a year. To help minimize corneal transplant complications and expedite healing, follow your eye surgeon’s instructions.
Trachea Transplantation
Trachea transplant helps the patients suffering from hardening and narrowing of their windpipe. It also repairs surgical defects of the laryngotracheal airway tract.
Revascularization of the trachea, is considered as the first towards a fruitful tracheal transplantation, and the only way to that at the moment is wrapping the isolated trachea with a well- vascularized soft tissue flap perfused by a vascular pedicle. It is then possible to transfer the revascularized trachea to an airway defect.
Skin Grafting
Skin grafting is an effective treatment option for patients suffering from deep burns, skin infections, bed sores, open wounds, and skin cancer surgery.
In skin grafting procedure, the skin is removed from one area of the body, and moved or transplanted to a different area of the body where the skin has been lost.
Skin graft is performed under general anesthesia, using two basic types including: split-thickness and full-thickness grafts.
In split-thickness grafting the top layer of the skin –the epidermis- along with a deeper layer of the skin –dermis- is removed from the donor site, which is usually taken from outer thigh, abdomen, buttocks, or back, transplantation takes place. These grafts are used to cover large areas.
In full-thickness grafting all of the epidermis and dermis are removed from the donor site. These grafts are usually taken from abdomen, groin, forearm, or collarbone, and are used to cover smaller areas like small wounds or highly visible parts of the body.
It is noted that full-thickness grafts have a better cosmetic result as they blend in well with the skin around them.
Before the surgery tell your doctor about any medications you are taking, as some certain medicines interfere with blood’s ability to form clots. It is also recommended to stop smoking for weeks before the surgery to expedite the healing process.
The procedure is performed under general anesthesia. After removing skin from the donor site, your surgeon will carefully place it over the transplant area, and then secures it with surgical dressing to prevent contamination or further trauma to the wound.
It is noted that developing blood vessels and connecting to the skin around the graft should normally start within 36 hours.
It is usually recommended to stay at the hospital for a few days after a split-thickness graft to make sure the healing process is going well. You also need to avoid doing any kind of activities that includes stretching or injuring the graft site.
It is noted that skin can be recovered within 15 hours of a donor’s death, and stored at very cold temperatures for many years.
Multivisceral Organ Transplants
In this type of transplant more than one organ is transplanted. Based on patient’s condition these transplants may include combinations like heart/lung, heart/kidney, or kidney/pancreas transplants.
Bone Graft
Bone grafting, or bone transplant, is a surgical procedure used to fix problems with bones or joints. Bone graft is beneficial in case of multiple fractions, in regenerating bone lost to disease, infection, or injury, and in helping to heal around surgically implanted devices, like joint replacements.
The bone for a bone graft can come from:
• Your body such as your ribs, hips, pelvis, or wrist, called autograft,
• Or a deceased donor, called allograft,
• Or be completely synthetic.
The type of graft depends on the type of your injury, and the injured part of the body. For example, allografts are commonly used in hip, knee, or long bone reconstruction like arms and legs. It is noted that in bone graft in this type the risk of infection is lower.
It should also be noted that the risk of rejection compared to organ transplants is minimal since allograft bone transplant involves bone that has no living cells. Also, there is no need to match blood types between the donor and the recipient since the transplanted bone does not contain living marrow.
The procedure is performed under general anesthesia. Your surgeon then will make incisions in the skin above where the graft is needed, and then shape the (donated) bone to fit the area. The graft will be held in place using pins, plates, screws, wires, or cables. After closing the incision with stitches and binding the wound, a cast or splint may be used to support the bone while it heals.
Recovery can take from two weeks to more than a year. You should avoid heavy physical activity for as long as your surgeon suggests.
During your recovery, keep your arm or leg above the level of your heart. You should also exercise the muscle groups that weren’t affected by the surgery to help you keep your body in good shape. To expedite the healing procedure it is recommended to quit smoking.
After an Organ Transplant
It feels euphoric to wake up after the surgery and find those symptoms gone. Anesthesia protects you from post-surgical pain for a short time. To make the overall experience as comfortable as possible, follow your surgeon’s instructions.
It is highly recommended to stay organized with an organ transplant care checklist. This list will be helpful in keeping track of appointments, scheduling for medications, diet, and exercising.
To recover fully and return to a normal active lifestyle involves taking sensible steps. Working closely with your transplant team plays an active role in your recovery.
You need to change your diet after transplant, and also drink more water. You will also need to get laboratory tests done frequently.
You can also resume your activities that you had to give up because of your illness. However, do not resume any activity without getting approval from your doctor.
Anti-rejection medicine reduces your immune system ability to reject a transplanted organ by weakening or reducing your immune responses to foreign material. Meanwhile these drugs allow you to maintain enough immunity to prevent infection.
Before taking any new medicine check with your transplant team.
Replace any soft, sticky, hard, cracked medicine or any medicine with a notably different color or odor.
It is very helpful to communicate with your friends, family, and your caregiver.
To prevent infection:
• Make sure you stay away from anyone who is sick, including your loved ones.
• Be cautious and hygienic around pets.
• Consistently wash your hands thoroughly with soap and water.
• Instead of reusable wash clothes, use disposal paper towels.
• Follow additional specific guidelines your transplant team instructs you.
It is also important to help your family member or friend (who has gone through transplant surgery) to stay strong and persist through challenges. Try to remain calm, patient, and understanding through difficult moments your loved ones go through. These difficult moments including mood swings or outbursts during moments of frustration, stress, or sadness could simply be reactions to certain medications.
In order to be at your best physically and mentally, it is important to take good care of yourself. Get adequate rest, nutrition, and exercise.
